WHO changes COVID-19 vaccine recommendation for pregnant women
LOS ANGELES - The World Health Organization has changed its guidance on whether pregnant women can safely take a COVID-19 vaccine.
The organization previously warned pregnant women against receiving the Moderna vaccine, originally saying the vaccine was "currently not recommended" for pregnant women unless they are at high risk of exposure.
Now, the agency says, "Based on what we know about this kind of vaccine, we don’t have any specific reason to believe there will be specific risks that would outweigh the benefits of vaccination for pregnant women."
The WHO added that there is very little data available to them to assess safety for pregnant women surrounding the COVID-19 immunization.
"Those pregnant women at high risk of exposure to SARS-CoV-2 (e.g. health workers) or who have comorbidities which add to their risk of severe disease, may be vaccinated in consultation with their health care provider," the WHO said.
Responding to the WHO’s original recommendation earlier this week, the American College of Obstetricians and Gynecologists (ACOG) previously said neither COVID-19 vaccine should be withheld from pregnant women, and that women should discuss individual risks and benefits with their health care providers.
RELATED: Study suggests severe COVID-19 among pregnant women raises risk of preterm birth, death link
The Society for Maternal-Fetal Medicine (SMFM) has also recommended that the new mRNA COVID-19 vaccines be offered to pregnant and breastfeeding individuals.
"As physicians who care for pregnant individuals, and as vaccine rollout expands to other eligible populations, ACOG and SMFM continue to firmly assert that pregnant individuals should be given the opportunity to make their own decision as to whether to receive the COVID-19," according to a joint statement by the ACOG and SMFM.
The U.S. government’s emergency authorization for the Pfizer and Moderna vaccines doesn’t list pregnancy as a reason to withhold the shots.
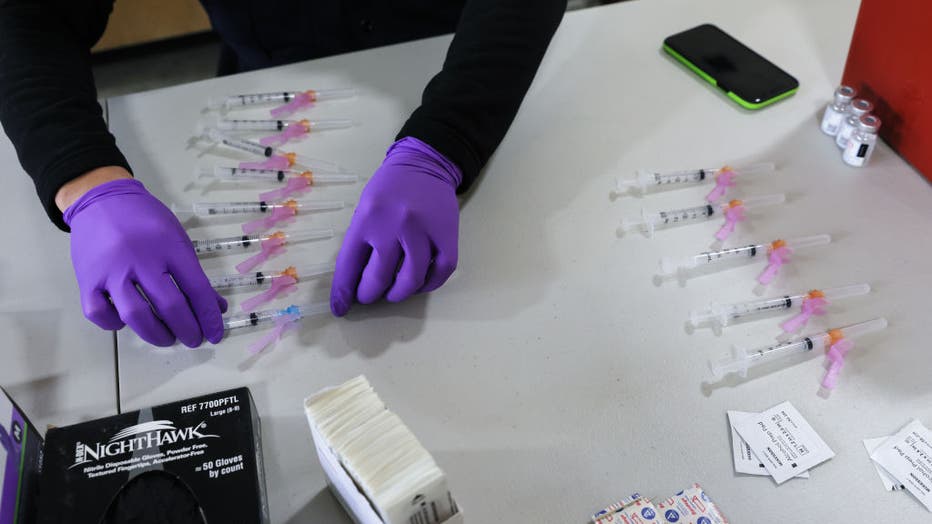
A firefighter paramedic prepares COVID-19 vaccination doses at a Los Angeles Fire Department (LAFD) fire station on January 29, 2021 in Los Angeles, California.
But the OB-GYN groups both say women should consult their doctors, since COVID-19 vaccines have not yet been tested in pregnant women. Evidence about safety and effectiveness is reassuring from studies that inadvertently included some women who didn’t know they were pregnant when they enrolled.
The U.S. Centers for Disease Control and Prevention on Monday also revamped its list of which Americans are at high risk for severe COVID-19 illness, adding pregnant women.
Pregnant women joined the list on the same day a CDC report found they accounted for about 9% of lab-confirmed COVID-19 cases in women of childbearing age. About 5% of women of childbearing age are pregnant at any given time.
The report showed that pregnant women had higher rates of hospitalization, of admission to a hospital intensive care unit and of winding up on a breathing machine vs. young women who weren’t pregnant. There was no clear evidence of a higher death rate among pregnant women, however.
It’s not completely surprising, said Dr. Denise Jamieson, chair of obstetrics and gynecology at the Emory University School of Medicine. Pregnant women have been found to be at higher risk from other infectious respiratory diseases, likely because the lungs decrease in the volume as the uterus grows, Jamieson said.
What is surprising, she said, is that the CDC didn’t place pregnant women in the highest risk category.
"To me this is the most compelling evidence to date that pregnant women are at increased risk," said Jamieson, who spent 20 years at CDC as a reproductive health expert.
Earlier this week, CDC officials called on a panel of experts to help them identify groups that should be prioritized for coronavirus vaccinations if one becomes available and supplies are limited.
Pregnant women could be among that group. So could certain racial and ethnic groups.
A new study suggests pregnant women who contract severe COVID-19 disease face a heightened risk of death and preterm delivery compared to those with asymptomatic cases of the illness.
However, the study’s lead author said adverse outcomes were not associated with mild-to-moderate coronavirus infections.
"Our research shows that serious pregnancy complications appear to occur in women who have severe or critical cases of COVID and not those who have mild or moderate cases," Dr. Torri D. Metz, a maternal-fetal medicine subspecialist and associate professor at the University of Utah Health, said in a related news release.
Findings were presented Thursday at a virtual meeting for the Society for Maternal-Fetal Medicine, according to a news release from the National Institutes of Health, which funded the study.
The study follows previous findings from the CDC, which said pregnant women who contract the coronavirus are more at risk for severe illness and death than non-pregnant women.
The CDC said pregnant women should be counseled about the importance of seeking prompt medical care if they develop symptoms of coronavirus, and that there should be a strong emphasis on coronavirus prevention for pregnant women at each medical appointment.
The Associated Press contributed to this story.

