Wisconsin psychiatric bed shortage magnified by spike in competency orders
Wisconsin psychiatric bed shortage
A FOX6 investigation found an explosion in court-ordered competency treatment is pushing state mental hospitals beyond their limits.
WAUKESHA, Wis. - A FOX6 investigation found an explosion in court-ordered competency treatment is pushing state mental hospitals beyond their limits.
That revelation emerged from a felony case that offers a rare glimpse into the inner workings of the state's forensic mental health system.
"Are you continuing to take your medication?" asked Judge Michael Bohren, as he addressed a defendant in his courtroom.
"Um, I went, um…" began Timothy Hoeller, before the judge cut him off.
"I asked you are you continuing to take your medication?" Bohren asked a second time.
Hoeller is facing felony charges for making "terrorist threats" against his former employer, Carroll University. The charged were filed in February 2022. Since then, Hoeller's fitness to stand trial has been a key issue in the case.
If Hoeller would accept psychiatric treatment voluntarily, his brother, Daniel Hoeller, said he probably wouldn't be dealing with criminal courts at all.

Timothy Hoeller tells a Waukesha County judge he's stopped taking psychiatric medications after his release from involuntary competency restoration.
"If he could get on a good regimen of prescriptions," Dan Hoeller said, "he’d be fine."
His father, 96-year-old Don Hoeller, said he might be better off in a mental health institution: "Be better for society."
But Hoeller's stay at a state mental hospital earlier this year was brief. And in an August court hearing, Judge Bohren tried to determine if he was continuing to follow a regiment of psychiatric treatment.
"So you’re not taking medications," Judge Bohren asked.
"I'm not taking cholesterol lowering, blood pressure or psychiatric medications," Hoeller replied.
SIGN UP TODAY: Get daily headlines, breaking news emails from FOX6 News
Hoeller's family members said they don't know what else to do.
"Is jail the right place for somebody like your brother?" FOX6 Investigator Bryan Polcyn asked.
"I don’t know," Daniel Hoeller said. "I think that’s about the only thing you can do at that point."
At 62 years old, Timothy Hoeller has a severe case of bipolar disorder that has landed him in and out of jails and mental hospitals in Illinois and Wisconsin. He's been accused of bombarding the courts with frivolous lawsuits and scaring government employees and university administrators with references to mass shootings. He once called a Florida school shooter his "hero."
Hoeller's most recent charges stem from his own personal feud with Carroll University, which fired him from a part-time physics teaching job in 2017. After his termination, Hoeller made repeated references to homicide, suicide and school shootings in correspondence with the university and others. The writings prompted the school to issue a campus wide safety alert.

In February 2022, Waukesha Police Det. Kenny Stucker interviewed Hoeller about the references to mass violence.
"He then indicated that Carroll University's methods are the reason people shoot up universities and schools," Stucker testified in May 2023.
But Hoeller's court-appointed attorney, Paul Crawford, said the words were not intended as an actual threat.
"Does he say he’s going to do that?" Crawford asked.
"He references it," Stucker replied.
"How? Where does it say in that line that he’s going to do this?" Crawford asked.
"He doesn’t say he’s going to do it," Stucker replied. "But he’s making reference to it, which would make any reasonable person from the community fear for their safety."
FREE DOWNLOAD: Get breaking news alerts in the FOX6 News app for iOS or Android
But this is about more than one man with a troubled mind. It's about a mental health system in crisis.
"It is not a situation that any of us wants to be in," said Anne Bensky, deputy chief legal counsel for the Wisconsin Department of Health Services, testifying before Judge Bohren in November 2022. "The department is doing everything it can."
Hoeller was born in 1961. One year earlier, the U.S. Supreme Court issued a landmark decision – Dusky v. United States – that guarantees criminal defendants the right to a competency evaluation before they go to trial.
Hoeller's attorney asked for just such a review last fall. When a forensic psychologist found him not competent, Hoeller objected. It set up a rare, but fully public, contested competency hearing.

Jenna Niess, forensic psychologist, testifies in Timothy Hoeller's November 2022 competency hearing
"Mr. Hoeller is substantially lacking in his mental capacity to understand the proceedings," testified Jenna Niess, a forensic psychologist who evaluated Hoeller for the state.
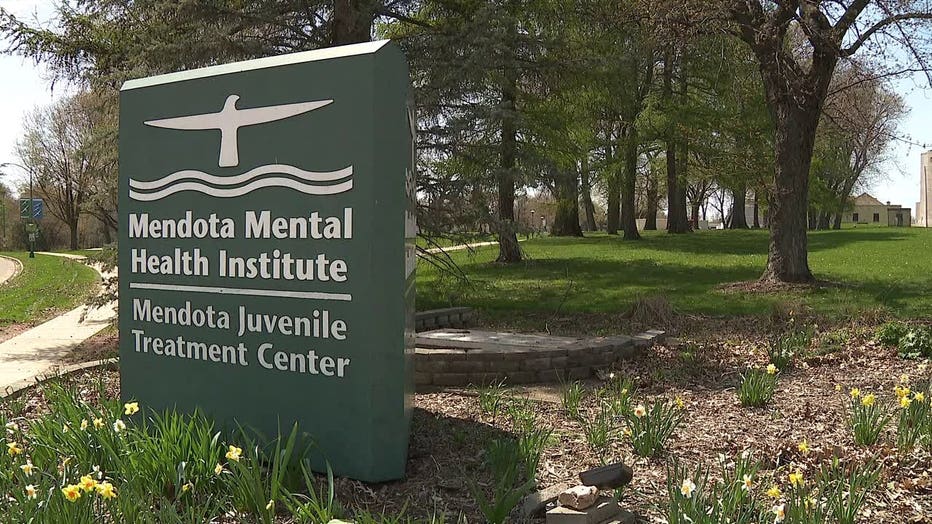
Based on her testimony, among others, Judge Bohren placed the criminal case on pause and ordered Hoeller to be committed to Mendota Mental Health Institute (MMHI).
The judge's order directed the state of Wisconsin to treat Hoeller until he could be deemed fit for trial, a process known as "treatment to competency," or TTC.
"We’ve wanted help," Don Hoeller said. "And we got help."
Instead of going to directly to Mendota, however, Hoeller spent weeks sitting in the Waukesha County Jail.
"He was stuck down there for at least a month," Don Hoeller said.
Why? Because jails have space that the state's forensic psychiatric hospital does not.
Gregory Van Rybroek, Director of Mendota Mental Health Institute, testifying in December 2022
"There is a significant waiting list to get into Mendota," Bensky said.
"I think that’s an inherent insult to the public and to the state of Wisconsin," Bohren said.
One month after the commitment order, Hoeller was still 70th on a list of 109 male patients waiting for a bed to open up. The judge called state officials into court to explain the delay.
"His case ruffled some big people down at Mendota," Don Hoeller said.
"This is very common in the United States," said Gregory Van Rybroek, director of MMHI. "It’s part of a nationwide trend."
Van Rybroek said, in recent years, they've seen a sharp rise in court orders for forensic evaluation and treatment.
Competency evaluations are up 59% since 2016 and TTC orders have increased 150%. Meanwhile, the available bed space for forensic psychiatric patients has only increased 23% in the time. In other words, the system is vastly over capacity. The state has no choice but to prioritize the sickest, most dangerous patients first.
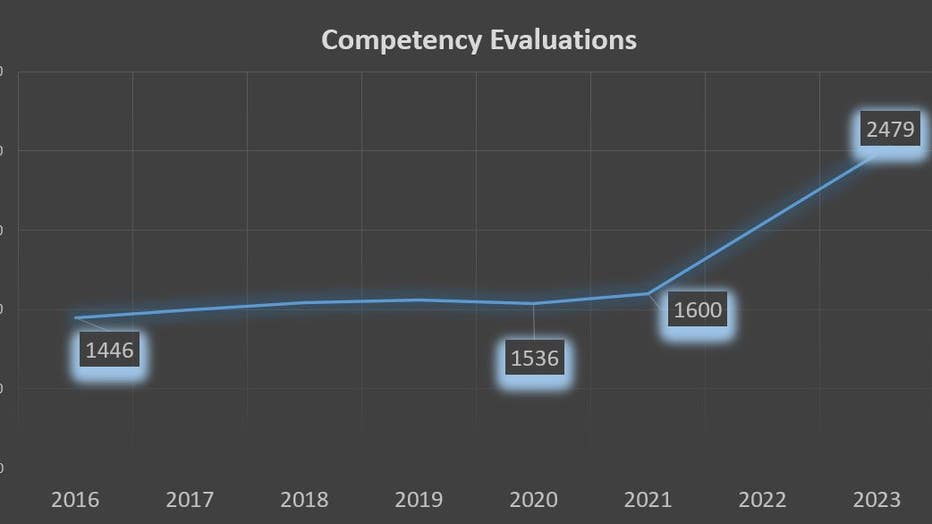
Source: Wisconsin DHS data obtained through open records
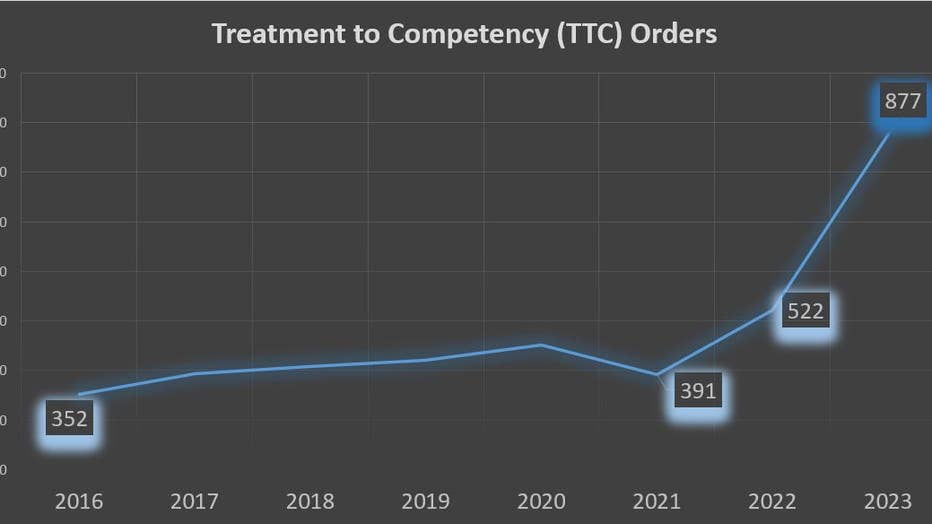
Source: Wisconsin DHS data obtained through open records
"Self abusive, fecal smearing, fecal eating, smashing ones head against the wall or the door," he said.
"There is such a backlog of people that need that treatment," said Dr. Tony Thrasher, a board certified psychiatrist and spokesperson for the Wisconsin branch of NAMI, the National Alliance on Mental Illness.
Thrasher said it's not just state mental hospitals that lack bed space, but private ones, too: "Very few hospitals in the area have psychiatric capacity."
A 2021 study by reseachers at Salem State University found Wisconsin is one of 28 states with a shortage of psychiatric beds. The study's analytical model shows Wisconsin needs 248 more inpatient psychiatric beds to meet the need – a need increase of 17%.
But Dr. Thrasher said what's actually happening is the opposite. For example, Froedtert Hospital in Menomonee Falls recently closed its inpatient psychiatric unit.
"There have unfortunately been more and more closures than there have been openings," Dr. Thrasher said, "so what was already a precarious position is worsening."
"It is a statewide issue," said Dodge County Sheriff Dale Schmidt.
Schmidt said the burden for filling that gap often falls to law enforcement, especially when they're called to help with a person experiencing a mental health crisis.
"We are transporting them in a cage in the back of a squad car between these facilities," Schmidt said.
Last year, Dodge County deputies spent more than 269 hours transporting people in a mental health crisis to hospitals, where deputies stand guard until the patient is medically cleared to be transferred to a psychiatric facility. Then, the deputies drive even farther to find a facility willing to take them.
"We’re spending hundreds of dollars, sometimes thousands of dollars, on a case just trying to get somebody in front of a mental health provider," Schmidt said.
Sometimes, they end up going to jail instead, because the legal threshold for a criminal detention is lower.

Dodge County Sheriff Dale Schmidt says a lack of psychiatric beds is causing his deputies to spend long hours standing guard at hospitals and transporting individuals in a mental health crisis
"I think law enforcement is often left with an uncomfortable choice," Dr. Thrasher said.
"They sit in jail," Schmidt said, "mentally ill, with nobody to help them for weeks and weeks until we can get them there."
When they finally do get into treatment, they don't necessarily stay there long.
"They just filled him up with some kind of prescription," Dan Hoeller said. "Made him really a zombie."
Timothy Hoeller spent about two months in Mendota before doctors cleared him for release in February with a high-dose prescription for Resperdal, an anti-psychotic medication.
"He was literally just quiet, stiff, rigid," Dan Hoeller said. "Wouldn’t say much, talk much. No emotion. No affect."
Hoeller's criminal case resumed. Soon, he stopped taking medications again.
"I was taking psychiatric medication," Timothy Hoeller said. "That I got off of."
FREE DOWNLOAD: Get breaking news alerts in the FOX6 News app for iOS or Android.
"He was real agitated yesterday after court," Daniel Hoeller said. "Got home and started writing all these missives again."
According to Dr. Thrasher, that is not unusual: "Just because you were treated to competency in the hospital doesn’t mean you will then maintain on that regimen or be forced to maintain on that regimen."
What is unusual is how often people like Timothy Hoeller are getting sent back to the state for repeated competency treatment. In 2016, DHS said just 14 people ordered to undergo competency restoration in Wisconsin were repeat clients. In 2022, that figure was 163. It's a 1,064% increase in repeat TTC orders in just six years.
"Wow, that's a sobering number," Dr. Thrasher said. "I think this speaks to a larger, systemic problem."
And solving that problem will take commitment.
FOX6 Investigators asked the director of MMHI, Gregory Van Rybroek, for an on camera interview three times. He did not respond. Instead, the Wisconsin Department of Health Services declined an interview on his behalf, writing that the doctor is "extremely busy."
In an email to the FOX6 Investigators, DHS Communications Specialist Elizabeth Goodsitt writes:
"As for the answer to your question about whether declining the interview is a matter of timing or topic, I can tell you, the answer is both. As you can imagine, Greg is extremely busy and does not have a lot of availability. And at this point, we will not be able to allow a crew on campus.
Also, we know you have been delving into this issue for a while and we appreciate that. But we are concerned you may not be allowed the time to devote to the nuances and complexities of this topic. We are happy to continue working with you to get some questions answered in writing ahead of a future interview, but I am unable to get one on the books at this time."
Goodsitt did respond to a series of written questions. Here are the questions, as well as her responses:
- How many total psychiatric inpatient beds are there, currently, at MMHI? 308 beds (16 civil geriatric beds; the remaining 292 are forensic beds)How many total beds does DHS have statewide? 492 beds (this includes beds at MMHI and WMHI. this does not include beds at Mendota Juvenile Treatment Center (max of 29 beds). MJTC serves boys who do not respond to the rehabilitation services provided at Wisconsin’s youth correctional institution.*Based on bed availability, there are two other DHS operated facilities that could potentially serve another 80 forensic patients. These 80 beds are not included in the total bed count of 492. Can you break these down by type (adult vs. juvenile, male/female/coed, forensic/civil)? This often varies based on needs within the institutes, particularly related to civil patients. For example, a civil geriatric patient may not be admitted to a geriatric-specific bed based on bed availability. The following totals include WMHI and MMHI combined. Please note – some of these patients are counted more than once. For example, an adult male forensic patient is counted in the forensic, male, and adult categories. Forensic patients ~336.Civil patients ~156.Adult patients ~450 (does not include 16 geriatric patient beds)Youth patients ~55 (includes MJTC beds)Geriatric ~16Male and female beds are fluid based on need.
- The 2023-25 biennial budget signed by Governor Evers appears to include $10-million in supplemental appropriations for regional Crisis Urgent Care and Observation Facilities. Can you tell me the current status of any plans DHS is aware of to build or fund regional crisis urgent care and observation facilities in Wisconsin? If such plans exist, where would those facilities be located? How many inpatient psychiatric beds would they have?Gov. Evers’ 2023-2025 budget provides $10 million GPR over the biennium in the Joint Committee on Finance supplemental appropriation to establish up to two crisis urgent care and observation centers that will: • serve as regional crisis receiving and stabilization facilities; • offer seamless transitions between levels of services offered at the centers; • arrange for the transfer to more appropriate treatment options as needed; • coordinate the connection to ongoing care; and • promote the effective sharing of information between providers to improve service delivery and patient outcomesBeyond providing access to these additional services, the centers will help reduce the amount of time law enforcement and first responders currently must dedicate to emergency detention cases by offering a dedicated first responder drop-off location that accepts custody of emergency detention cases and does not require that medical clearances be completed before drop-off. DHS is working with the legislature to develop the framework for the crisis urgent care and observation centers.
- At a hearing in Waukesha County Criminal Case No. 2022CF345, DHS Deputy Chief Legal Counsel Ann Bensky told the court, "Despite very significant efforts from the department over the last several years to increase bed space, that hasn’t been able to keep up with the increased referrals for competency evaluations and treatment to competency." What specific efforts has DHS made over the last several years to increase bed space at Mendota?Please see the attached letter that was filed with the court in November 2021. A summary is below:Since 2016, through budget requests and other means, DHS has added 114 inpatient beds for treatment to competency and NGI (not guilty by reason of mental disease or defect) patients at Mendota. The 114 inpatient capacity was possible only through requests to renovate and repurpose buildings and hire more staff. Our ability to build, acquire, and staff facilities is governed by statute. Building and acquiring property is vested by statute not with DHS, but with the Department of Administration, the Building Commission, and the Governor. See Wis. Stat. §§ 13.48; 16.84(5); 20.867; 20.924(1)(b). State agency expenditures and staffing increases must be approved by legislative committee and the governor through the biennial budget process. See Wis. Stat. §§ 16.42-47; 16.505. Since the 2013-15 budget cycle, DHS has requested and received funding for capital renovations and staff at Mendota, which has resulted in 54 additional beds. In February 2018, DHS opened a vacant 20-bed unit at Sand Ridge Secure Treatment Center (SRSTC) to treat NGI patients, which freed up 20 more beds at Mendota for forensic admissions. In March 2020, DHS expanded its SRSTC operation by opening 20 more beds. To staff the SRSTC unit, the 2019-21 biennial budget provided DHS with 36.5 full-time equivalent (FTE) one-year project position authority. In addition to legislative initiatives, DHS has recently modified its operations at the Wisconsin Resource Center (WRC) by realigning staffing, occupancy and general operations to expand its current jail-based treatment to competency program by 25 beds.

