Patients, insurers say ambulance provider is overcharging: 'Outrageous'

Patients, insurers say ambulance provider is overcharging: 'Outrageous'
Patients floored. The ambulance company some say is really taking them for a ride.
LAKE GENEVA, Wis. - When taking a life-saving ambulance ride, you often don’t have time to ask questions.
Like, "what is this going to cost?" Or, "can I choose my provider?"
One woman wrote to Contact 6 about an ambulance provider she feels is overcharging for their services.
In early September, Christine Chialiva took a 42-mile ambulance ride between hospitals. She’d been staying in a Lake Geneva hospital after falling and puncturing her lung. The hospital arranged her transfer to a Rockford facility where she could undergo surgery. Chialiva says she was reluctant to make the trip.
"I didn’t want to go," said Chialiva. "I refused, and they said, ‘You can’t refuse. You need to go.’"
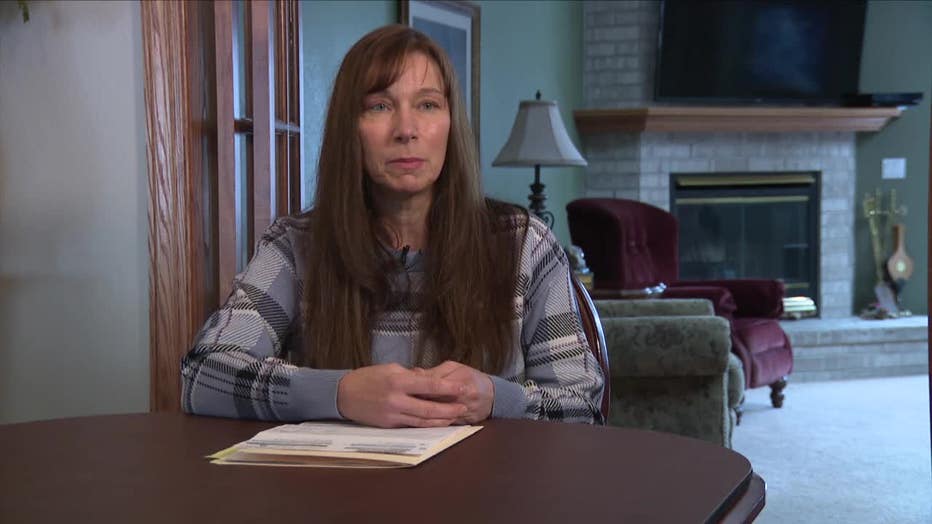
Christine Chialiva
In Rockford, Chialiva says she recovered without needing the surgery. A few months later, she got a bill from Superior Ambulance.
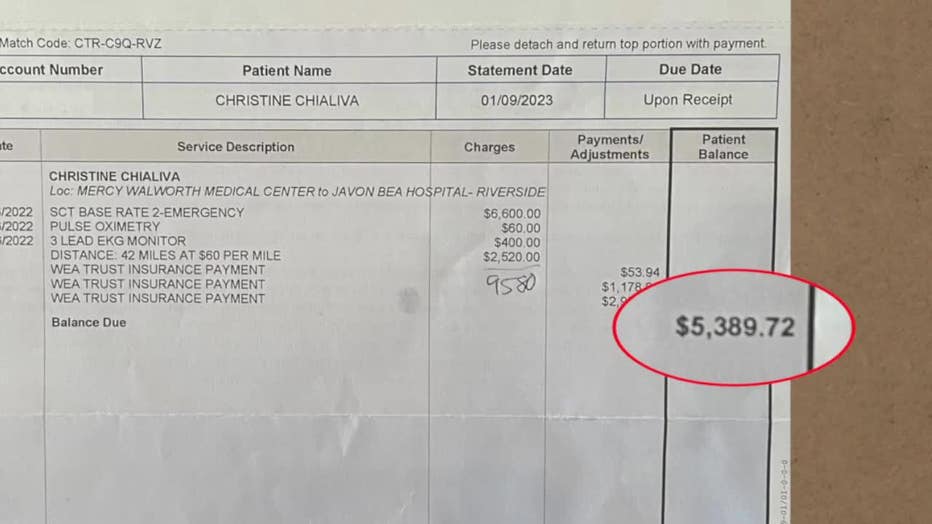
Superior Ambulance charged $9,580 for Chialiva’s ride. Her insurance provider at the time, the WEA Trust, covered $4,190. Chialiva owes Superior the remaining $5,390. So far, she’s held off on paying the bill. Last week, she got notice the bill is going to collections.
"I just feel like this bill is outrageous," said Chialiva.
SIGN UP TODAY: Get daily headlines, breaking news emails from FOX6 News
In general, when a patient has a health insurance plan, an ambulance company first sends its bill to the patient’s insurance provider. The insurance company sends payment for the amount it’s covering back to the ambulance company. The ambulance company then bills the patient for the remainder of their costs.

"There isn’t a hard and fast formula that [ambulance providers] use," said Maggie Adams, an EMS billing consultant with EMS Financial Services, Inc;, of calculating rates. "They all do it based on their own business needs."
Adams says many ambulance providers barely make ends meet due to high operations costs and difficulty retaining employees. There’s also the issue of low Medicare reimbursement rates, which Adams says are creating hardships for all operators.
"It has been such a hard-go for the industry," said Adams.

Maggie Adams, an EMS billing consultant with EMS Financial Services, Inc
It’s a struggle ambulance providers share, but Contact 6 found the billing is where Superior Ambulance stands apart.
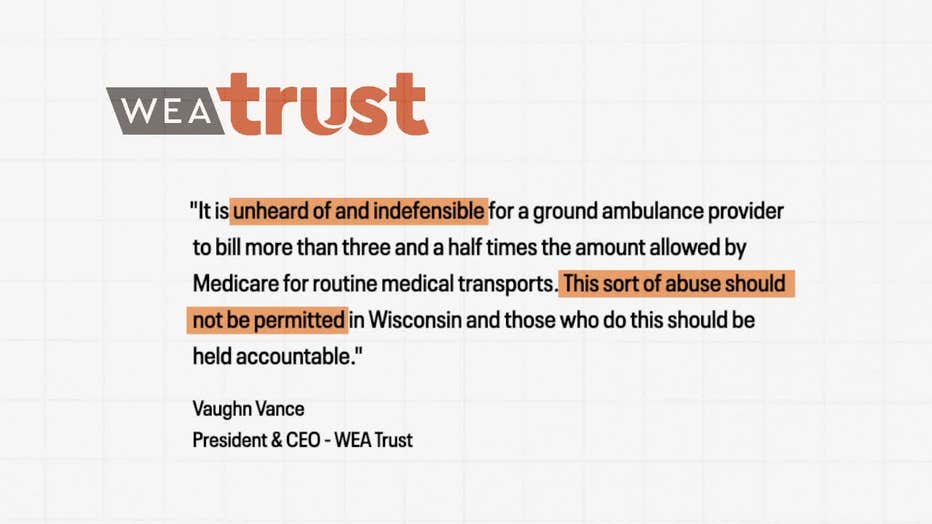
Chialiva says the WEA Trust told her they could not pay a higher portion of her bill, "because Superior’s charges were above anything reasonable." The WEA Trust reimbursed Superior Ambulance at a rate above what Medicare would cover.
"I definitely think Superior is wrong," said Chialiva.

Superior Ambulance
Ambulance providers designate Chialiva’s ride as ‘Specialty Care Transport,’ which is a transfer between medical facilities at the highest level of care they can provide, also referred to as "critical care."
Vaughn Vance, the President and CEO of WEA Trust, calls Chialiva’s bill from Superior Ambulance, "unheard of and indefensible."
"This sort of abuse should not be permitted in Wisconsin and those who do this should be held accountable," said Vance, in a statement sent to Contact 6.
The WEA Trust sent Chialiva a list of claims from other Wisconsin ambulance companies for Specialty Care Transport. The data shows most billed less than $3,000 or $4,000 for the rides. Superior Ambulances billed about $6,000 and higher.
Contact 6 also solicited base rates for Specialty Care Transport from other Wisconsin ambulance providers. LifeStar reported a base rate of $2,400. Orange Cross said it charges $1,915.48. Bell Ambulance reported $2,270. MMT said its base rate is $2,016.
Chialiva’s bill reveals Superior Ambulance charged her $6,600 for Specialty Care Transport.

Superior Ambulance
Michael James got the same charge.
"I’m not disputing the service. I’m disputing the outlying cost," said James.
Back in May, Superior Ambulance transported James five miles between hospitals. It charged $7,705 for the ride. His insurance covered $1,791, leaving James to pay the remaining $5,914.
"When you’re in an emergency, you don’t have time to comparison shop for something that’s outside of insurance. You’re stuck," said James. "That’s exactly where I am. I’m stuck."

Michael James
Anthem Wisconsin, James’ insurer, agrees his charge is too high. In January, a spokesperson told Contact 6 it had asked Superior Ambulance "to waive the excessive charges". James says his bill remains unchanged.
Superior Ambulance exchanged emails with Contact 6 but did not go on camera.
"We cannot comment on the fees, tax subsidies, or payor mixes for other ambulance companies," wrote Mary Franco, Vice President of Superior Air Ground Ambulance Service Inc. "Superior stands behind our charges as they are necessary to provide competitive wages and benefits to our men and women who work long hours in stressful situations to serve our communities."
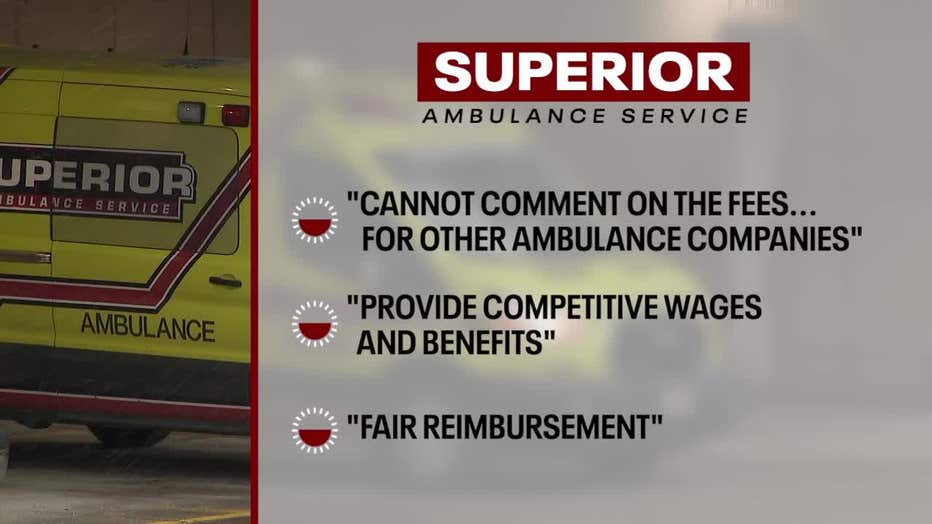
Franco also wrote, "Superior continues to attempt to work with the commercial payors for fair reimbursement to keep the patients out of the middle."
FREE DOWNLOAD: Get breaking news alerts in the FOX6 News app for iOS or Android
"The hospital usually calls the ambulance, so [patients] have no choice in the matter," said Steve Bernas, President and CEO of the Better Business Bureau (BBB) of Chicago.

Steve Bernas, President and CEO of the Better Business Bureau (BBB) of Chicago
Bernas says the BBB is looking into Superior Ambulance after getting 54 complaints about the Illinois-based company in two years. Last year, 24 of the 36 complaints the BBB received about Superior Ambulance were related to billing issues. The BBB says the remaining complaints were about service issues.
Also taking a closer look into Superior Ambulance is Wisconsin’s Department of Health Services, which cited an ongoing investigation in its denial of Contact 6’s open records request. Contact 6 asked to review complaints submitted about Superior Ambulance.

Superior Ambulance
In Wisconsin, there is no statewide regulation of ambulance rates, nor mandate that all health insurers provide coverage for the rides. Ambulance rides are also a notable exemption to the federal ‘No Surprises Act,’ which protects consumers from surprise medical bills.
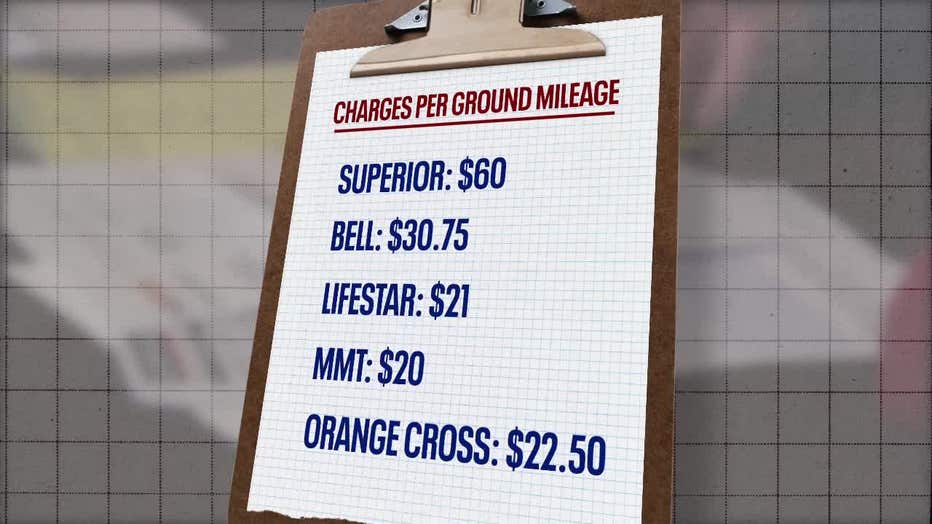
Contact 6 took a closer look at Chialiva’s and James’ bills from Superior Ambulance. It discovered Superior Ambulance also listed a charge of $60 per mile of transit. Other Wisconsin ambulance providers told Contact 6 they charge between $20 and $30.75 per mile of transit.
Mercyhealth arranged Chialiva's transfer with Superior Ambulance between its hospitals. It tells Contact 6 that Mercyhealth "cannot comment on any one particular patient or case," but confirms Mercyhealth has an agreement with Superior Ambulance.
"Although we can use any ambulance service available and we would like to provide a choice, hospitals are not always given that opportunity because there are very limited resources in Walworth County," said Kara Sankey, Mercyhealth Chief Nursing Officer and VP of Operations.
If you receive an ambulance bill you can’t pay, try calling the ambulance company and asking for a conference call with the billing department and your insurance provider. You may also qualify for the ambulance provider’s financial hardship program.
Full statement: Mary Franco, Superior Ambulance
"Ambulance providers, like Superior, are heavily regulated through state and local mandates which dictate the equipment we must have, staffing levels and the protocols for the care we provide. Ambulances along cost over $400,000 when full equipped and that is before wages, fuel and medication costs. We provide quality healthcare to patients when they are in need and when such care is prescribed by the patient’s physician.
"We cannot comment on the fees, tax subsidies or payer mixes for other ambulance companies, but Superior stands behind our charges as they are necessary to provide competitive wages and benefits to our men and women who work long hours in stressful situations to serve our communities.
"Superior is a small, family-owned company – Anthem and WA are respectively multi-billion/multi-million annual revenue corporations who choose to leave their patients to pay ambulance bills rather than providing full insurance coverage by negotiating fair reimbursement rates which ambulance providers which is why 80 percent of ambulance providers throughout the nation are out of network and which is why the US Congress excluded ambulance from the No Surprises Act.
"Superior continues to attempt to work with the commercial payers for fair reimbursement to keep the patients out of the middle."

